
Why rescheduling LSD and psilocybin would transform research into treating depression and anxiety
The UK Psychedelic Society has just launched a petition to reschedule LSD and psilocybin from Schedule I to Schedule II, so this seems like a great opportunity to explain what this means and why this is a good idea.
If you’ve been paying attention recently you’ll know we are in the midst of a Psychedelic Renaissance, discovering the clinical value of many psychedelic drugs. It’s early days, but if psychedelic-assisted treatment proves to be even half as effective as early clinical trials suggest, it will blow all existing treatments for depression, anxiety, addiction, and many other conditions out of the water.
The Research So Far
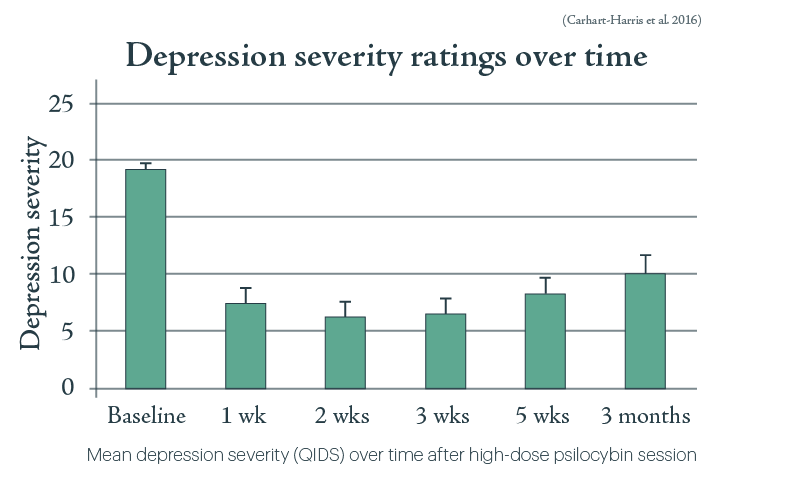
Last year, the Beckley/Imperial Research team gave a course of psilocybin-assisted therapy to twelve patients with treatment-resistant depression. 67% of patients reported a reduction in depression symptoms to non-clinical levels, one week after treatment; 42% remained in remission at 3 months without any further treatment. A follow-up study involving nineteen people was published by Imperial College researchers last week. By monitoring changes in brain activity, they found psilocybin ‘may effectively “reset” the activity of key brain circuits known to play a role in depression.‘ And this was in patients who had already shown no improvement from two or more anti-depressants. Yes, there was no placebo condition in the pilot trial, and it’s hard to blind patients from the effects of psychedelics anyway, but a much larger randomised controlled trial is now in the works.
Meanwhile, two separate research teams used LSD-assisted therapy to treat anxiety in cancer patients. Both of them saw a significant and sustained drop in anxiety levels, following exactly the same pattern.
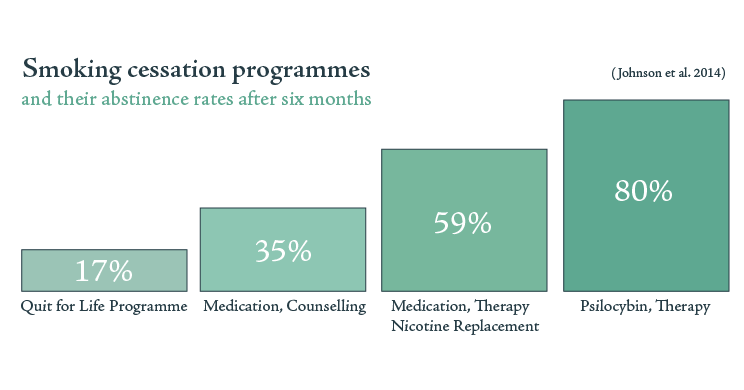
On top of that, the Beckley Foundation has been involved with a study at Johns Hopkins of psilocybin for smoking addiction. Chronic smokers, smoking an average of 19 cigarettes a day for 31 years, were given a 15-week Cognitive Behavioural Therapy course including three psilocybin sessions. 80% of this group were totally abstinent at a 6 month follow-up; those who had resumed smoking still showed a significant reduction in consumption. 12 months later, 67% of the group remained totally abstinent. In contrast, the most effective smoking cessation treatment outcome reports less than 31% abstinence after 12 months. We’re not the only ones looking at this; an NYU team used a similar programme to achieve a 27.2% decrease in drinking among chronic alcoholics; a level that was sustained until the final check-in at 36 weeks.
Research prior to 1971
But perhaps it’s harsh to condemn the UN scheduling system for not reflecting this research. These developments have all happened over the last five years, so none of this could have been known in the Seventies. Unfortunately, there’s a catch. None of this is recent news at all. LSD and psilocybin were both widely-used medicines when they were scheduled in 1971, and there was two decades’ worth of evidence demonstrating how safe and effective they were for clinical use. In fact, LSD had over 3,000 medical papers published about it, including an estimated 25,000 patients in total, making it arguably the most-researched psychoactive substance of all time.
To be sure, many of these are case studies, and reports that don’t meet today’s gold standard for clinical evidence. But recent literature reviews, focusing purely on high-quality randomised controlled trials, paint an extraordinary picture.
One such review looks at clinical trials of psychedelics for depression between the 50s and 70s. It finds 109 trials, though only 21 meeting the required level of quality. The reported improvement in these groups of depressed patients ranges between 40% and 95%. Another review focuses on LSD in the treatment of alcoholism, finding 6 proper randomised controlled trials from a total pool of 68 papers. Meta-analysis of these findings gave an odds ratio of 1.96, meaning that among the 536 patients treated in total, LSD treatment was almost twice is likely to lead to improvement as placebo.
LSD’s therapeutic power in addiction was known and utilized for decades. The founder of Alcoholics Anonymous was in fact one of its most prominent patients and supporters, attributing LSD with saving him from both alcoholism and depression.
So LSD and psilocybin weren’t placed on Schedule I due to lack of evidence of their therapeutic value. They were placed on Schedule I in the face of thousands of published scientific papers attesting to their therapeutic value, a move which was met with far more concerted opposition from scientists and psychiatrists than from hippies. Two decades’ worth of clinical research was first ignored and then forgotten; laboratories and careers were shut down; the War on Drugs claimed thousands of psychiatric patients as the first of its many civilian casualties.
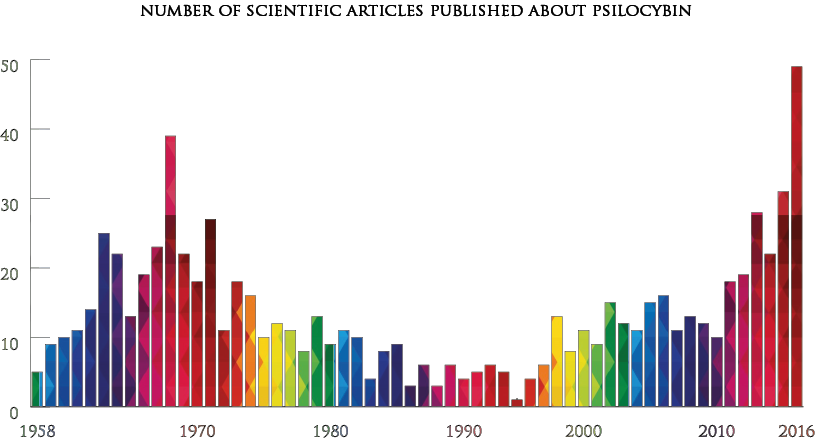
This figure includes clinical trials in humans, behavioural studies in animals, commentaries and review articles about psilocybin research. The results are drawn from a Pubmed keyword search for psilocybin.
‘A particularly serious problem to public health’
OK, but there’s more to being on Schedule I than therapeutic value. What about the other side of the cost/benefit coin; the risk of abuse and threat to public health? Was the loss of psychedelic medicine the price we simply had to pay to protect the public?
LSD and psilocybin happen to be among the least toxic psychoactive substances known to humanity; it’s easier to get a toxic reaction from water than from either substance.
As has been proved time and time again, neither LSD or psilocybin pose a risk of addiction; in fact, as we saw above, they’re probably the strongest weapons we have against drugs of abuse that are threatening public health, such as alcohol and tobacco. Contrary to popular belief, LSD and psilocybin don’t cause any risk of long-term psychosis or other mental health issues; in fact, two huge population analyses revealed that they were associated with an decrease in a number of markers of general mental illness including psychological distress, use of psychiatric medication, and inpatient and outpatient psychiatric intervention.
LSD and psilocybin use has been known to cause accidents, leading to injury or even death. But accidental injury and death is also possible while sober; we can only assess the psychedelic-induced risk by comparison with the baseline. If we do this, we discover that injury or death is unaffected by psychedelic use. This is why two major expert comparisons of recreational drug harms scored both LSD and psilocybin 0 on their ‘risk of physical harm caused by altered behaviour’ subscale. (Unsurprisingly, alcohol scores highest, by a country mile, on this particular measure.) The important factors determining your likelihood of an accident while tripping are the same as while sober: your tendency to take risks, your impulsivity, and so on.
So, LSD and psilocybin do not pose a risk of abuse, nor a threat to public health. In fact, if used correctly, they’re major assets to public health; the only thing stopping this is the drug scheduling laws themselves. All the recent evidence we discussed for the therapeutic value of LSD and psilocybin has been established by scientists who devoted years, if not decades, of their lives to re-opening this research field in the face of near-insurmountable legal obstacles. Scheduling laws, far from protecting public health, have been denying life-saving medication to patients suffering from depression, anxiety, addiction, and many other mental illnesses that we’ve not had a chance to discuss, for fifty years.
Current scheduling laws, in other words, have little to no therapeutic value and pose particularly serious problems to public health. These substances must be rescheduled urgently, to open the doors to research. From the evidence we’ve brought together today, LSD and psilocybin could be justifiably moved straight to Schedule IV, which contains substances far more dangerous and less therapeutically valuable than them. But Schedule II is a good start.
Convinced? Sign the petition.
Words: Dr. Alex O’Bryan-Tear
Podcast
- All
Links
- All
Support
- All
BIPRP
- All
Science Talk
- All
Amanda's Talks
- All
- Video Talk
- Featured
- 2016 Onwards
- 2011-2015
- 2010 and Earlier
- Science Talk
- Policy Talk
One-pager
- All
Music
- All
Amanda Feilding
- All
Events
- All
Highlights
- All
Psilocybin for Depression
- All
Current
- All
Category
- All
- Science
- Policy
- Culture
Substance/Method
- All
- Opiates
- Novel Psychoactive Substances
- Meditation
- Trepanation
- LSD
- Psilocybin
- Cannabis/cannabinoids
- Ayahuasca/DMT
- Coca/Cocaine
- MDMA
Collaboration
- All
- Beckley/Brazil Research Programme
- Beckley/Maastricht Research Programme
- Exeter University
- ICEERS
- Beckley/Sant Pau Research Programme
- University College London
- New York University
- Cardiff University
- Madrid Computense University
- Ethnobotanicals Research Programme
- Freiburg University
- Medical Office for Psychiatry and Psychotherapy, Solothurn
- Beckley/Sechenov Institute Research programme
- Hannover Medical School
- Beckley/Imperial Research Programme
- King's College London
- Johns Hopkins University
Clinical Application
- All
- Depression
- Addictions
- Anxiety
- Psychosis
- PTSD
- Cancer
- Cluster Headaches
Policy Focus
- All
- Policy Reports
- Advisory Work
- Seminar Series
- Advocacy/Campaigns
Type of publication
- All
- Original research
- Report
- Review
- Opinion/Correspondence
- Book
- Book chapter
- Conference abstract
- Petition/campaign
Search type




