Here’s How MDMA Treats PTSD
A military veteran suffering from Post-Traumatic Stress Disorder (PTSD) once described MDMA-assisted psychotherapy as “like years of therapy in two or three hours.” Yet despite the drug’s time-defying ability to accelerate mental and emotional healing, legislation regarding MDMA’s scheduling status has advanced at a glacial pace – until now. The FDA’s decision this month to designate the compound a ‘Breakthrough Drug’ could mark the beginning of a seismic shift in mental healthcare, and has paved the way for a Phase III clinical trial of MDMA for PTSD.
Carried out by a team of researchers from the Multidisciplinary Association for Psychedelic Studies (MAPS), the study will build on decades of evidence as to the potential of MDMA to facilitate psychotherapy. Ralph Metzner and Sophia Adamson wrote about the healing properties of the drug back in the 1980s, and provided a case study of a woman who, after being treated with MDMA, was finally able to overcome the trauma of being raped.
A decade later, George Greer and Requa Tolbert published a paper explaining how the drug helps patients to surmount the “subjective fear response to an emotional threat,” enabling them to face their traumatic memories and resolve internal conflicts. This idea was later reinforced by a study conducted by the Beckley/Imperial Research Programme, which found that the areas of the brain that process autobiographical memories exhibit a less severe response to negative memories when under the influence of MDMA.
While theories and protocols have varied over the years, one thing has remained constant: MDMA has never been considered a direct cure for PTSD in and of itself. Rather, it is used to help facilitate psychotherapy, enabling practitioners and patients to work together to overcome certain stumbling blocks on the path to recovery.
Julie Holland, the official medical monitor for MAPS’ clinical studies, summed this up in a recent interview in which she described MDMA as “a catalyst that’s used during therapy. It makes the therapy go deeper, it goes faster, it’s much more comfortable.”
This effect is thought to occur because of the way that MDMA interacts with neuroreceptor sites in the brain. For example, like many psychedelics, the drug causes an increase in serotonin, which helps to regulate mood and allows patients to stay calm, relaxed and grounded when faced with difficult memories or episodes.
MDMA also boosts oxytocin, which is sometimes referred to as ‘the love hormone’ because of the role it plays in fostering loving relationships and feelings of intimacy. It’s likely that this helps patients to form strong emotional bonds with their therapists, encouraging them to be more open and trusting in the way that they confide in them, while generating a sense of security.
Finally, the compound also produces an elevation in dopamine, leading to enhanced alertness and feelings of pleasure and reward, all of which assists patients in tackling and overcoming challenging mental situations and dilemmas.
Yet these are merely the broad brushstrokes of MDMA’s mode of action, and more research into the minutiae of the drug’s underlying neural mechanisms is required. For that reason, the Beckley Foundation is preparing to carry out a separate study on MDMA-assisted psychotherapy for PTSD at Cardiff University, which will examine the drug’s effect on activity within the amygdala – a brain region strongly associated with emotional processing.
PTSD is a notoriously difficult condition to treat, and is linked with an increased risk of depression and suicide, as well as substance abuse, inability to maintain employment and unstable relationships. In their recent Phase II clinical trial, MAPS administered three MDMA-assisted psychotherapy sessions to 107 patients with treatment-resistant PTSD, each of whom had suffered from the condition for an average of almost 18 years.
At the 12-month follow-up, an incredible 68% no longer qualified for a PTSD diagnosis. Speaking at Breaking Convention in London in June 2017, Holland described this statistic as “unheard of” in mental healthcare clinical trials.
If the Phase III results can replicate this then MDMA could become a life-saving medication for millions of people around the world within the next half decade.
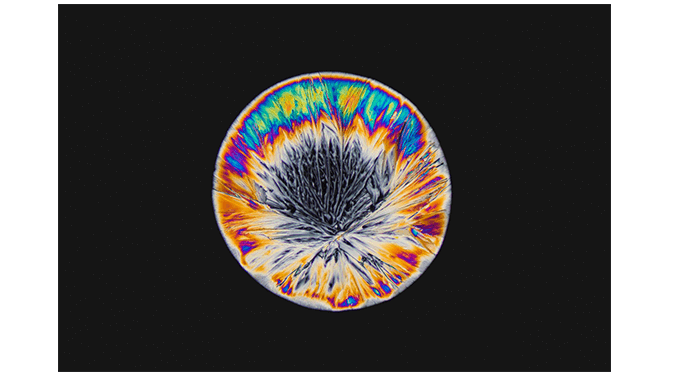
Main Image: an MDMA crystal under the microscope. Maurice Mikkers
Words: Benjamin Taub
Podcast
- All
Links
- All
Support
- All
BIPRP
- All
Science Talk
- All
Amanda's Talks
- All
- Video Talk
- Featured
- 2016 Onwards
- 2011-2015
- 2010 and Earlier
- Science Talk
- Policy Talk
One-pager
- All
Music
- All
Amanda Feilding
- All
Events
- All
Highlights
- All
Psilocybin for Depression
- All
Current
- All
Category
- All
- Science
- Policy
- Culture
Substance/Method
- All
- Opiates
- Novel Psychoactive Substances
- Meditation
- Trepanation
- LSD
- Psilocybin
- Cannabis/cannabinoids
- Ayahuasca/DMT
- Coca/Cocaine
- MDMA
Collaboration
- All
- Beckley/Brazil Research Programme
- Beckley/Maastricht Research Programme
- Exeter University
- ICEERS
- Beckley/Sant Pau Research Programme
- University College London
- New York University
- Cardiff University
- Madrid Computense University
- Ethnobotanicals Research Programme
- Freiburg University
- Medical Office for Psychiatry and Psychotherapy, Solothurn
- Beckley/Sechenov Institute Research programme
- Hannover Medical School
- Beckley/Imperial Research Programme
- King's College London
- Johns Hopkins University
Clinical Application
- All
- Depression
- Addictions
- Anxiety
- Psychosis
- PTSD
- Cancer
- Cluster Headaches
Policy Focus
- All
- Policy Reports
- Advisory Work
- Seminar Series
- Advocacy/Campaigns
Type of publication
- All
- Original research
- Report
- Review
- Opinion/Correspondence
- Book
- Book chapter
- Conference abstract
- Petition/campaign
Search type