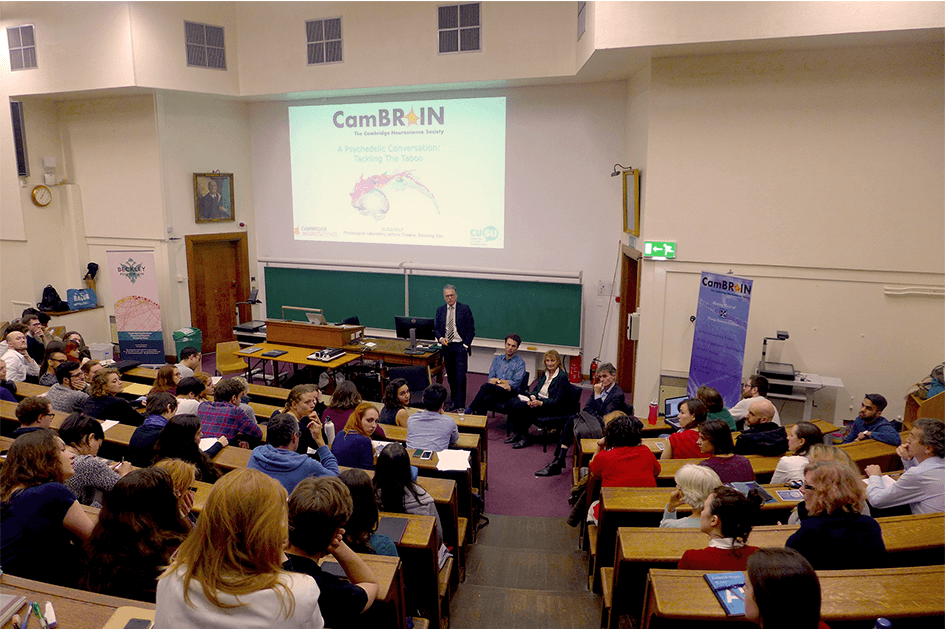
A Psychedelic Conversation at Cambridge University
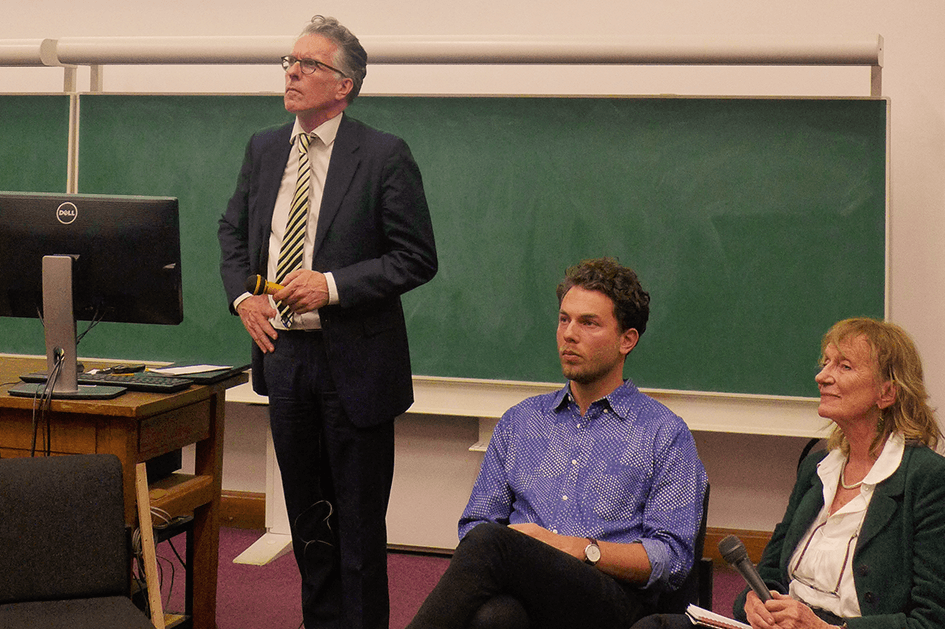
‘A Psychedelic Conversation: Tackling the Taboo’ was an apt title for Tuesday night’s proceedings, hosted by the Cambridge Neuroscience Society. Amanda Feilding, Professor Paul Fletcher of the Cambridge psychiatry department, and Leor Roseman of the Beckley/Imperial Research Programme all drew on their individual areas of expertise to make the case for just how valuable psychedelics are to science and medicine.
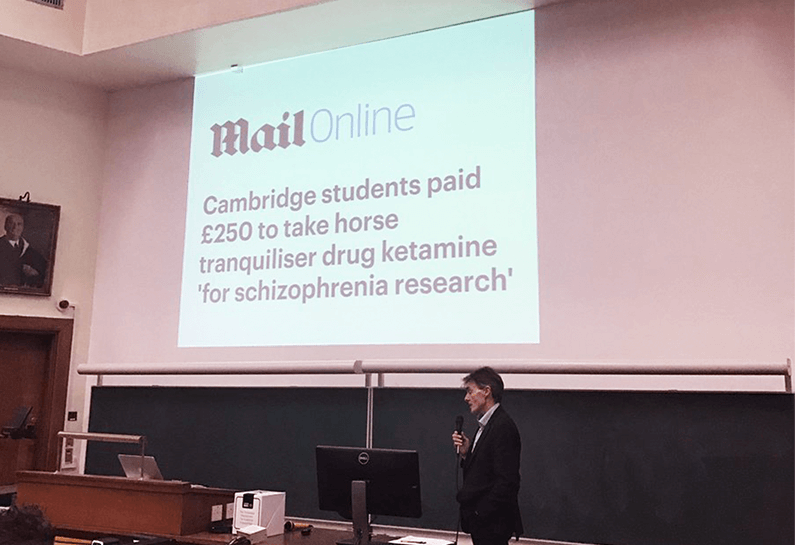
First to speak was Paul Fletcher, who explained how mind-altering substances – in this instance ketamine – can be incredibly useful as a model of psychosis. This is because some of ketamine’s effects bear significant neurological and behavioural similarities with the early stages of psychosis.
Professor Paul Fletcher on the usefulness of ketamine as a model for understanding psychosis – and the Daily Mail’s reaction to his research
Models are indispensable tools for scientific research, but when it comes to stigmatized substances like psychedelics, the media often seems to forget (or ignore) the fact that a model is just that – a model. Fletcher pointed out that you wouldn’t look through the windows of a prototype aeroplane and complain that you couldn’t see a pilot or a working drinks trolley. A model should only be judged on the purpose it serves, and in the case of early stage psychosis, ketamine serves this purpose very well.
It is substances such as ketamine that have the potential to help psychiatrists leap across what Paul Fletcher called the ‘explanatory gap’: scientists can explain the neural mechanisms of what happens when someone is suffering from psychosis, but not how this then translates into a psychotic experience – such as the belief that the TV is talking to you personally.
Amanda Feilding took the conversation on from here, with her talk, emphasising how recent scientific studies with psychedelics are on track to create a new psychiatry, ‘not only in how we treat, but also in how we understand psychological disorders.’ Amanda’s full talk, ‘Opening the Doors to Psychedelic Medicine’, can be read below. In reframing the dialogue about psychedelics, Amanda proposed that psychedelics should be ‘conceived as non-specific medicines for a wide range of disorders.’ Recent research collaborations from the Beckley Foundation combatting alcohol and smoking addiction, treatment-resistant depression, and cluster headaches all demonstrate the far-reaching potential of psychedelics as a therapeutic tool.
It was a point that would come up again and again throughout discussion, so it was fitting that the final question of the evening came back round to it:
‘What is the common mechanism whereby it is logical to think the psychedelic agent will have efficacy in such a range of diverse symptoms? What’s the driving mechanism?’
Amanda replied, ‘I think it’s breaking free of constrictions which keep the thought patterns and behaviours patterns rigid. They break down – we see that in brain imaging – and that shapes the rigidity of the setting and gets to the deeper level of the core of the person, so that if they are in a therapeutic setting they react more to that person and they form new thoughts and new reactions to that situation.’
Leor Roseman spoke passionately about why he believes psychedelic therapy is so effective, and why it sits in such a stark contrast to the current status quo of anti-depressant prescriptions. SSRIs, the most common form of anti-depressants, follow a model of ‘chronic administration’, leading to an ‘emotional blunting’ in patients. Psychedelic therapy does the opposite by giving patients the capacity to confront and work through their emotions: where anti-depressants promote avoidance and disconnection, psychedelic therapy promotes acceptance and reconnection.
In the Q&A afterwards – chaired by the Cambridge Head of Psychiatry, Professor Ed Bullmore – the speakers had a frank discussion about the placebo problem in psychedelic research, the point at which research into meditation intersects with psychedelics, and the next steps in psychedelic research. As ever more research is carried out in the coming years, the findings will undoubtedly raise as many questions as they do answers, but the more we understand, the better the questions we can ask.
Words: Sasha Frost
The event was held on 21/02/2017 at Cambridge University, and was hosted by CamBRAIN, the Cambridge Neuroscience Society.
‘Opening the Doors to Psychedelic Medicine’ by Amanda Feilding
Podcast
- All
Links
- All
Support
- All
BIPRP
- All
Science Talk
- All
Amanda's Talks
- All
- Video Talk
- Featured
- 2016 Onwards
- 2011-2015
- 2010 and Earlier
- Science Talk
- Policy Talk
One-pager
- All
Music
- All
Amanda Feilding
- All
Events
- All
Highlights
- All
Psilocybin for Depression
- All
Current
- All
Category
- All
- Science
- Policy
- Culture
Substance/Method
- All
- Opiates
- Novel Psychoactive Substances
- Meditation
- Trepanation
- LSD
- Psilocybin
- Cannabis/cannabinoids
- Ayahuasca/DMT
- Coca/Cocaine
- MDMA
Collaboration
- All
- Beckley/Brazil Research Programme
- Beckley/Maastricht Research Programme
- Exeter University
- ICEERS
- Beckley/Sant Pau Research Programme
- University College London
- New York University
- Cardiff University
- Madrid Computense University
- Ethnobotanicals Research Programme
- Freiburg University
- Medical Office for Psychiatry and Psychotherapy, Solothurn
- Beckley/Sechenov Institute Research programme
- Hannover Medical School
- Beckley/Imperial Research Programme
- King's College London
- Johns Hopkins University
Clinical Application
- All
- Depression
- Addictions
- Anxiety
- Psychosis
- PTSD
- Cancer
- Cluster Headaches
Policy Focus
- All
- Policy Reports
- Advisory Work
- Seminar Series
- Advocacy/Campaigns
Type of publication
- All
- Original research
- Report
- Review
- Opinion/Correspondence
- Book
- Book chapter
- Conference abstract
- Petition/campaign
Search type